Radiofrequency tumor ablation system with a wireless or implantable probe
-
1.
School of Electrical and Computer Engineering, The University of Georgia, Athens, GA 30602, USA
-
2.
Center for Interventional Oncology, Radiology and Imaging Sciences, NIH Clinical Center, National Institute of Biomedical Imaging and Bioengineering, and National Cancer Institute Center for Cancer Research, National Institutes of Health, Bethesda, MD, USA
-
3.
Department of Biomedical Engineering, National University of Singapore, Singapore, Singapore
-
4.
Department of Electronic Engineering, University of York, Heslington, York, UK
More Information
-
Author Bio:
 Julian Moore
Julian Moore obtained his graduate and undergraduate education in electrical engineering at the University of Georgia. He is currently working at the Johns Hopkins University Applied Physics Laboratory in Maryland.
 Sheng Xu
Sheng Xu is the head scientist of the Center for Interventional Oncology at the National Institutes of Health. He obtained his PhD from the Department of Computer Science in the Johns Hopkins University. Then he worked at Philips Research North America for 6 years before he joined NIH. Dr. Xu is interested in surgical navigation, medical image processing, medical robotics and machine learning.
 Bradford Wood
Bradford Wood has practiced and performed translational research at NIH for the past 18 years with the goal of combining drugs devices, and image guidance to meet clinical needs. As an academic interventional radiologist, he defines clinical scenarios where combining image guidance and energy and drug deposition may lead to improved outcomes for cancer patients. He is the first to treat kidney cancer, lymphoma, adrenocortical carcinoma, and pheochromocytoma with radiofrequency ablation, first to combine heat deployed nanoparticle chemotherapy with RFA or HIFU thermal ablation, and first to use fusion guidance for biopsy and thermal ablation. He directs a multidisciplinary research team networking with the NIH institutes while partnering with drug device and pharma industry as well as extramural academic centers in the US and Europe.
 Hongliang Ren
Hongliang Ren is an IEEE senior member and currently serves as an associate editor for IEEE Transactions on Automation Science & Engineering (T-ASE) and Medical & Biological Engineering & Computing (MBEC). He has navigated his academic journey through Chinese University of Hong Kong, Johns Hopkins University, Children's Hospital Boston, Harvard Medical School, Children's National Medical Center, United States, and National University of Singapore. His areas of interest include biorobotics, intelligent control, medical mechatronics, soft continuum robots, soft sensors, and multisensory learning in medical robotics. He is the recipient of NUS Young Investigator Award and Engineering Young Researcher Award, IAMBE Early Career Award 2018, Interstellar Early Career Investigator Award 2018, and ICBHI Young Investigator Award 2019.
 Zion Tsz Ho Tse
Zion Tsz Ho Tse received his PhD in mechatronics in medicine from Imperial College London. Currently he is a chair professor at Department of Electronic Engineering and the principal investigator of the Medical Robotics Lab at University of York, UK. Before joining University of York, he was an associate professor in University of Georgia, USA. Dr. Tse has been involved in designing and prototyping a broad range of novel analog-digital electronic devices, most of which have been applied in numerous clinical and industrial environments
-
Corresponding author:
Zion Tsz Ho Tse, Department of Electronic Engineering, University of York, Heslington, York, UK. E-mail: zion.tse@york.ac.uk
-
Abstract
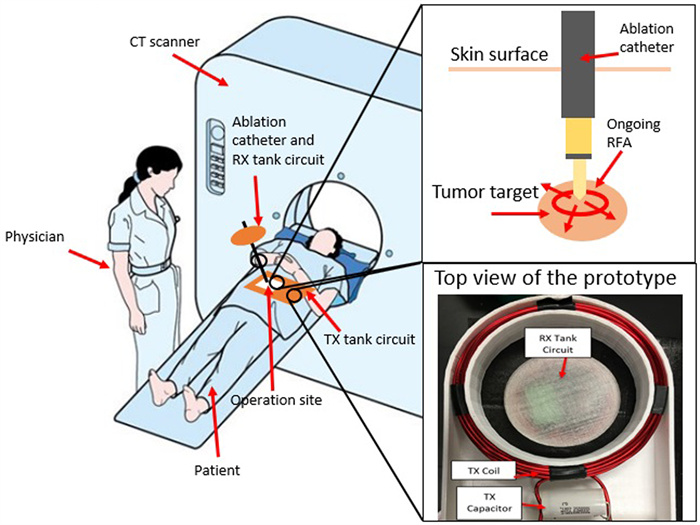
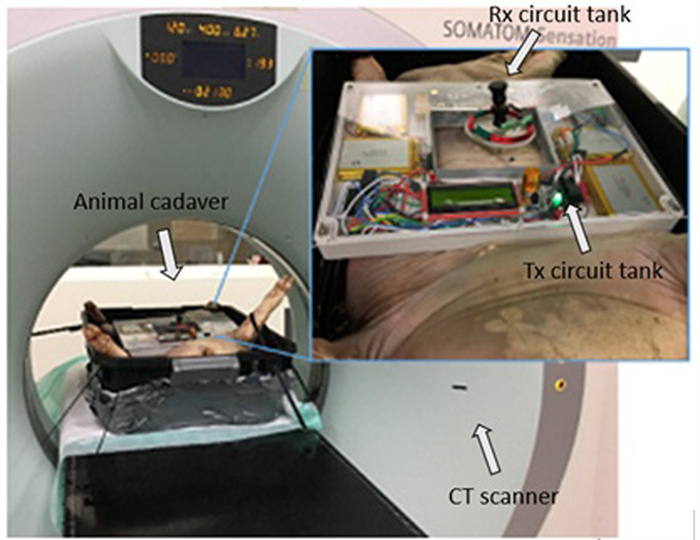
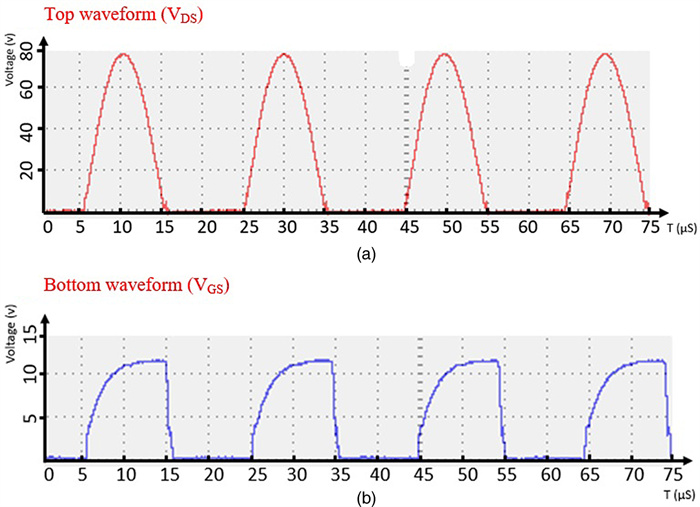
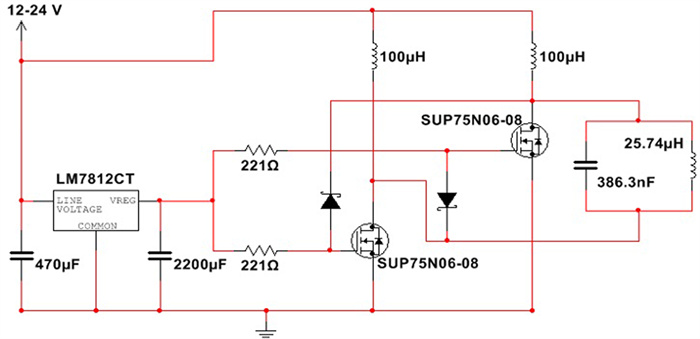
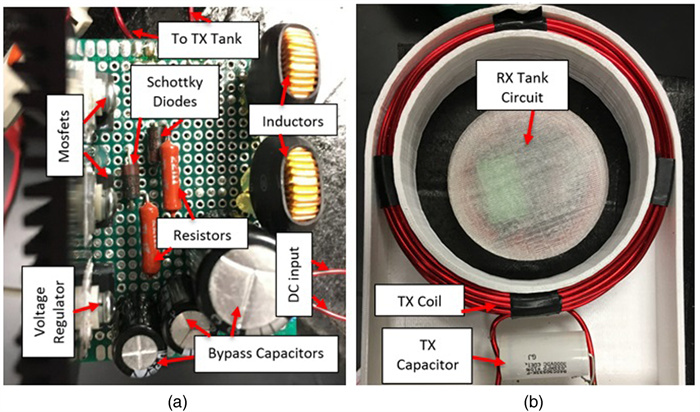
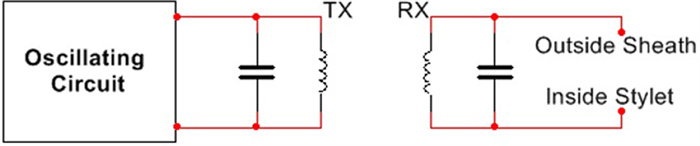
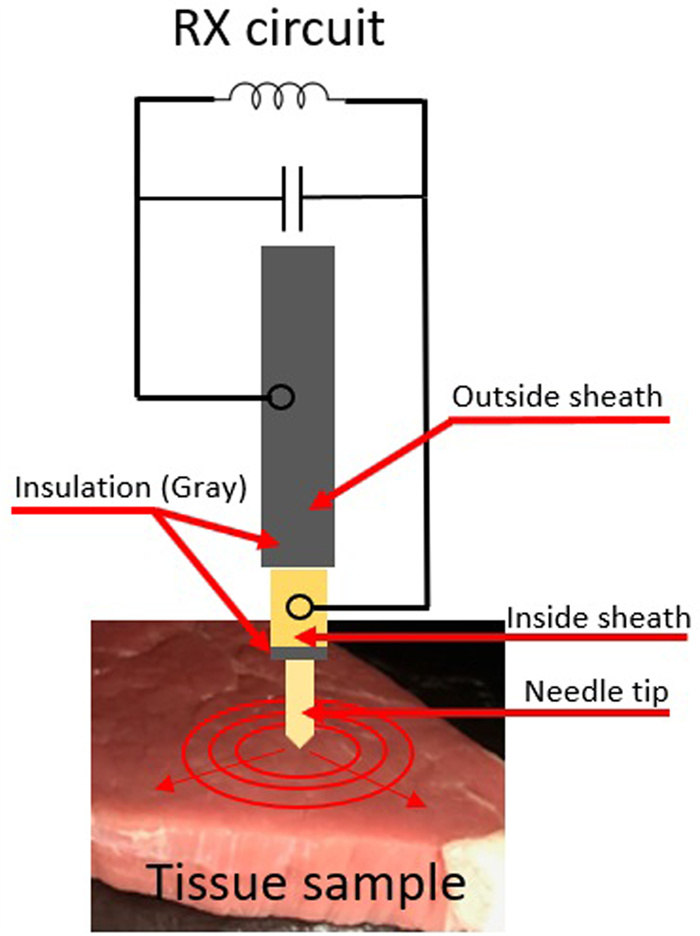
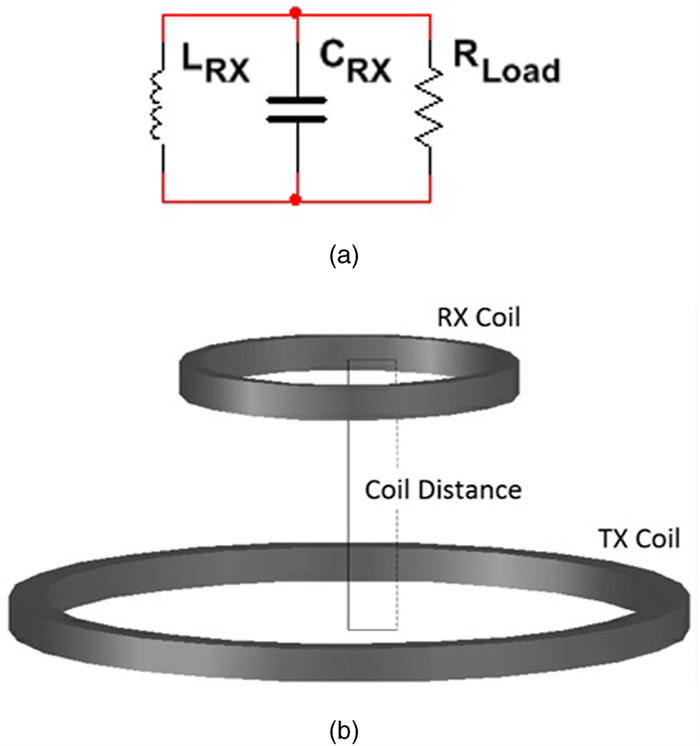
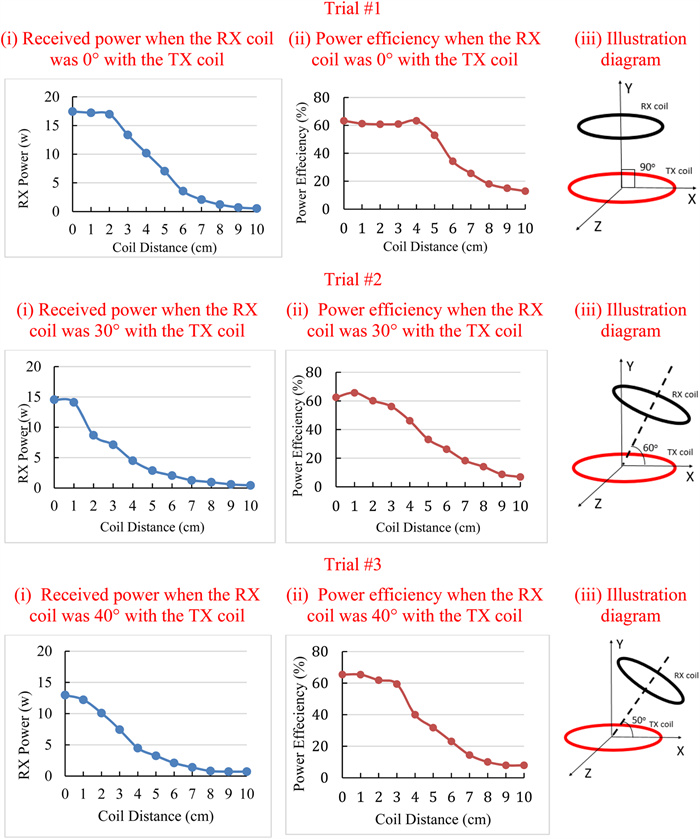
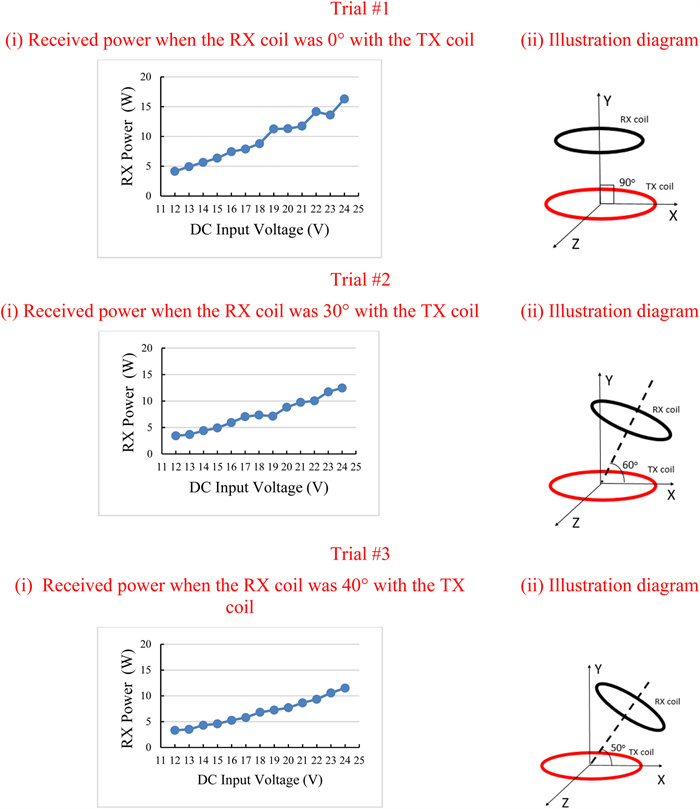
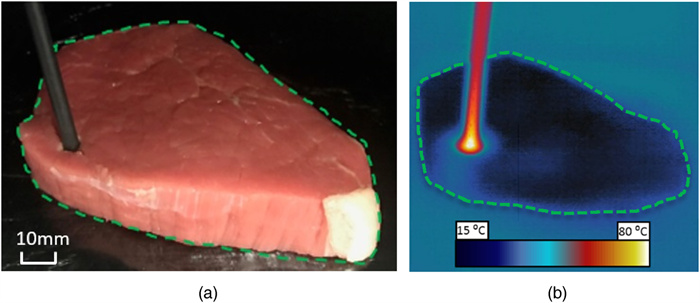
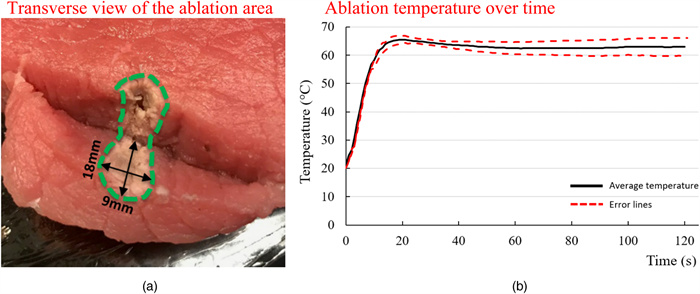
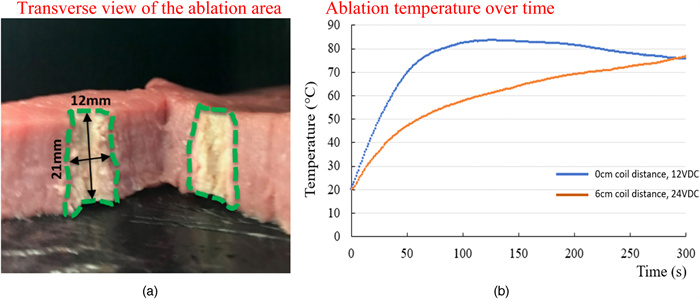
Radiofrequency ablation (RFA) is a non-invasive image-guided procedure where tumors are heated in the body with electrical current. RFA procedures are commonly indicated for patients with limited local disease or who are not surgical candidates. Current methods of RFA use multiple cords and wires that ergonomically complicate the procedure and present the risk of cutting or shorting the circuit if they are damaged. A wireless RFA technique based on electromagnetic induction is presented in this paper. The transmitting and receiving coils were coupled to resonate at the same frequency to ensure the highest power output. The receiving coil was connected to two insulated electrodes on a catheter, which allowed the current to flow to the targeted tissue. The prototype system was tested with ex-vivo bovine tissue, which has similar thermal and electrical properties to human tissue. The setup can monitor the received power, efficiency, temperature, and ablation zone during ablation procedures. The maximum received power was 15 W, and the average maximum efficiency was 63.27%. The novel system was also able to ablate up to a 2 cm ablation zone in non-perfused tissue. This proof of concept for performing RFA wirelessly with electromagnetic induction may merit further optimization.
-
About this article
Cite this article
Moore J, Xu S, Wood B J, Ren H, Tse Z T H. 2020. Radiofrequency tumor ablation system with a wireless or implantable probe. Wireless Power Transfer 7(2): 95-105 doi: 10.1017/wpt.2020.10
|
Moore J, Xu S, Wood B J, Ren H, Tse Z T H. 2020. Radiofrequency tumor ablation system with a wireless or implantable probe. Wireless Power Transfer 7(2): 95-105 doi: 10.1017/wpt.2020.10
|









 Julian Moore obtained his graduate and undergraduate education in electrical engineering at the University of Georgia. He is currently working at the Johns Hopkins University Applied Physics Laboratory in Maryland.
Julian Moore obtained his graduate and undergraduate education in electrical engineering at the University of Georgia. He is currently working at the Johns Hopkins University Applied Physics Laboratory in Maryland.  Sheng Xu is the head scientist of the Center for Interventional Oncology at the National Institutes of Health. He obtained his PhD from the Department of Computer Science in the Johns Hopkins University. Then he worked at Philips Research North America for 6 years before he joined NIH. Dr. Xu is interested in surgical navigation, medical image processing, medical robotics and machine learning.
Sheng Xu is the head scientist of the Center for Interventional Oncology at the National Institutes of Health. He obtained his PhD from the Department of Computer Science in the Johns Hopkins University. Then he worked at Philips Research North America for 6 years before he joined NIH. Dr. Xu is interested in surgical navigation, medical image processing, medical robotics and machine learning.  Bradford Wood has practiced and performed translational research at NIH for the past 18 years with the goal of combining drugs devices, and image guidance to meet clinical needs. As an academic interventional radiologist, he defines clinical scenarios where combining image guidance and energy and drug deposition may lead to improved outcomes for cancer patients. He is the first to treat kidney cancer, lymphoma, adrenocortical carcinoma, and pheochromocytoma with radiofrequency ablation, first to combine heat deployed nanoparticle chemotherapy with RFA or HIFU thermal ablation, and first to use fusion guidance for biopsy and thermal ablation. He directs a multidisciplinary research team networking with the NIH institutes while partnering with drug device and pharma industry as well as extramural academic centers in the US and Europe.
Bradford Wood has practiced and performed translational research at NIH for the past 18 years with the goal of combining drugs devices, and image guidance to meet clinical needs. As an academic interventional radiologist, he defines clinical scenarios where combining image guidance and energy and drug deposition may lead to improved outcomes for cancer patients. He is the first to treat kidney cancer, lymphoma, adrenocortical carcinoma, and pheochromocytoma with radiofrequency ablation, first to combine heat deployed nanoparticle chemotherapy with RFA or HIFU thermal ablation, and first to use fusion guidance for biopsy and thermal ablation. He directs a multidisciplinary research team networking with the NIH institutes while partnering with drug device and pharma industry as well as extramural academic centers in the US and Europe.  Hongliang Ren is an IEEE senior member and currently serves as an associate editor for IEEE Transactions on Automation Science & Engineering (T-ASE) and Medical & Biological Engineering & Computing (MBEC). He has navigated his academic journey through Chinese University of Hong Kong, Johns Hopkins University, Children's Hospital Boston, Harvard Medical School, Children's National Medical Center, United States, and National University of Singapore. His areas of interest include biorobotics, intelligent control, medical mechatronics, soft continuum robots, soft sensors, and multisensory learning in medical robotics. He is the recipient of NUS Young Investigator Award and Engineering Young Researcher Award, IAMBE Early Career Award 2018, Interstellar Early Career Investigator Award 2018, and ICBHI Young Investigator Award 2019.
Hongliang Ren is an IEEE senior member and currently serves as an associate editor for IEEE Transactions on Automation Science & Engineering (T-ASE) and Medical & Biological Engineering & Computing (MBEC). He has navigated his academic journey through Chinese University of Hong Kong, Johns Hopkins University, Children's Hospital Boston, Harvard Medical School, Children's National Medical Center, United States, and National University of Singapore. His areas of interest include biorobotics, intelligent control, medical mechatronics, soft continuum robots, soft sensors, and multisensory learning in medical robotics. He is the recipient of NUS Young Investigator Award and Engineering Young Researcher Award, IAMBE Early Career Award 2018, Interstellar Early Career Investigator Award 2018, and ICBHI Young Investigator Award 2019.  Zion Tsz Ho Tse received his PhD in mechatronics in medicine from Imperial College London. Currently he is a chair professor at Department of Electronic Engineering and the principal investigator of the Medical Robotics Lab at University of York, UK. Before joining University of York, he was an associate professor in University of Georgia, USA. Dr. Tse has been involved in designing and prototyping a broad range of novel analog-digital electronic devices, most of which have been applied in numerous clinical and industrial environments
Zion Tsz Ho Tse received his PhD in mechatronics in medicine from Imperial College London. Currently he is a chair professor at Department of Electronic Engineering and the principal investigator of the Medical Robotics Lab at University of York, UK. Before joining University of York, he was an associate professor in University of Georgia, USA. Dr. Tse has been involved in designing and prototyping a broad range of novel analog-digital electronic devices, most of which have been applied in numerous clinical and industrial environments