Introduction: Gastrointestinal cancers have a strong association with splanchnic vein thrombosis (SVT), yet the hospitalization data is unknown.
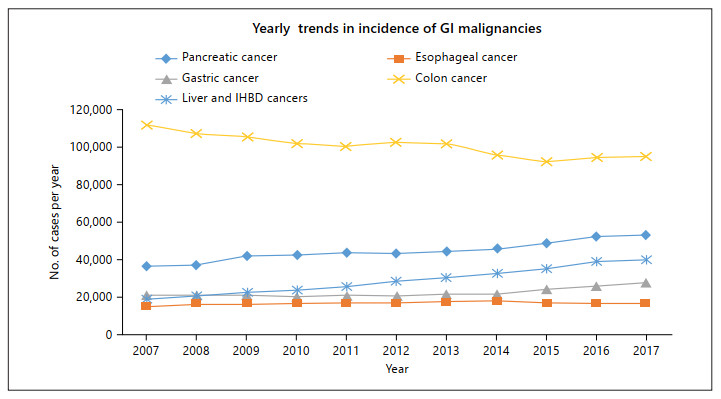
Objective and Methods: We analyzed around 78 million discharges from the 2007–2017 Nationwide Inpatient Sample with an inclusion criterion of adult patients admitted for portal or hepatic vein thrombosis as a primary diagnosis with a gastrointestinal or hepatobiliary malignancy as a secondary diagnosis. The outcomes were in-hospital mortality, complication rates, and resource utilization. Odds ratios (OR) and means were adjusted for confounders using multivariate regression analysis models.
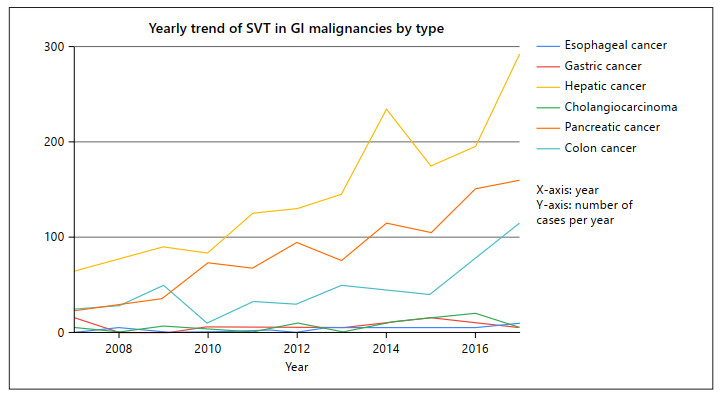
Results: Out of the total 32,324 hospitalizations for SVT, 3,220 (10%) were associated with a GI malignancy, of which hepatocellular carcinoma (HCC) and pancreatic cancer were the most common. Portal vein thrombosis accounted for 95% of these hospitalizations. Admissions for pancreatic cancer-associated SVT have increased by 7.2 times from 2007 to 2017. Patients with SVT and concomitant GI malignancies were significantly older and had a higher comorbidity score than those with SVT without GI malignancy. Risk of inpatient mortality for SVT patients were significantly higher for patients with gastric cancer (rate: 12.1%, OR 8.6, 95% CI: 1.8–39.7) and HCC (rate: 7.6%, OR 2.77, 95% CI 1.5–4.8) as compared to non-GI malignancy-related SVT. Odds of variceal bleeding were significantly higher for patients with HCC (OR 1.67, 95% CI: 1.2–2.34) than patients without GI malignancy.
Conclusions: Digestive cancer-associated SVTs constitute 10% of all SVT related hospitalizations and are significantly increasing in the past decade. We report the baseline characteristics and predictors of inpatient mortality in this study.